Amid the Omicron surge in New York City, a Bronx-based medical resident spoke with Left Voice about how the Covid-19 pandemic exposed long-standing issues in the U.S. healthcare system, why Biden’s blaming the unvaccinated is a problem, and what a socialist healthcare system could look like.
What has Covid-19 been like at your hospital since the Omicron surge? And in the Bronx more broadly?
Omicron swept through New York City rapidly. It was first identified in late November, and a month later, cases in New York City began to skyrocket, with projections literally looking like a vertical line. At that time, the severity of the variant was unclear, and we know from the first wave and the Delta wave that hospitalization rates increase after infectivity rate, and death rates come after that. For Omicron, our hospital had already initiated mobilization plans by late December. Our Covid-19 hospitalizations increased by 10-fold between mid-late December and now — but that includes patients who are being admitted for Covid-19 and those who are being admitted for other medical problems but just happen to test positive for Covid-19. Our epidemiologists also predicted 1,200 hospitalizations by mid-January, and the projections looked scary — it was a vertical line up. This brought up a lot of traumatized feelings among the residents, who are the main supply of labor for the hospital — because it felt like March/April 2020 again with the overwhelming number of patients being admitted for Covid-19, most of whom are disproportionately impacted because the communities we serve are poor, Black, and Brown. Thankfully, and to much surprise, however, we reached a plateau as of last week. Cases are not actually rising in a vertical line anymore — we reached a plateau and are hoping this continues and then eventually decreases. This means that Omicron is probably not as severe as Delta or the original coronavirus strain — especially for vaccinated individuals. For the unvaccinated, it’s a different story. The last I heard, half of the ICU was full of Covid-19 patients, and most of those were unvaccinated.
Right now, most of our medicine inpatient floors are full of Covid-19 patients — most of whom are being managed for respiratory distress. We have also deployed a few additional medical teams to assist with the increased load of hospitalization. This means that residents from other fields like psychiatry, pediatrics, and others have been pulled off their typical rotations to staff teams dedicated to treating Covid-19 hospitalizations. For example, part of the pediatric hospital has been converted to an adult Covid-19 ward. And my colleagues in psychiatry have been pulled off their rotations to work on Covid-19 teams.
As far as I can tell, the NYC Department of Health reports that the Bronx reached its peak of Omicron cases shortly after New Year’s — at about 8,300 positive cases — and the case positivity rate has decreased since then and continues on a steady decline. I remember seeing long lines at Urgent Cares around the holidays for people waiting to get tested. Lines would be wrapping around the block as early as 7:30 a.m., and the Urgent Cares wouldn’t even be open by then! But oddly enough, it felt like business moved as usual in the Bronx. I see a lot of people wear masks, and in my own primary care clinic, lots of patients came in with Covid-like symptoms and tested positive after we swabbed them — but many of the ones I saw were vaccinated, about half boosted, and they had only mild symptoms. At first we were worried we should convert all our patient care sessions to telemedicine, but that doesn’t seem necessary — we all take precautions in the clinic, and our patients do too.
Have increased Covid-19 cases affected care for patients presenting for things other than Covid?
So far, I don’t think it has. I’m on a rotation in my hospital where I interact a lot with surgical teams, and many are still proceeding with emergent, urgent, and elective surgeries even if patients are positive for Covid-19. This is different from the first wave, where all surgeries were canceled and all kinds of doctors and specialists mobilized to assist with the mass hospitalizations that ensued. Even in the outpatient setting, patients are coming in for routine visits, and we’re able to provide that for them.
The Omicron surge has been a good opportunity to talk about vaccinations with my patients — and several have gotten their boosters and others their first dose.
What are the working conditions at your hospital like?
Ooof. This question has many long answers. They aren’t good and never work. For the longest time it has felt like everything in the hospital is breaking down and we’re just waiting for the day when the building will collapse, which is really ironic because our hospital possesses millions and millions and spends a lot of money on public relations and hospital expansion. This means that our advertisements about our hospital can be seen across New York City and we’re continually acquiring new properties in the area. But inside the hospital, we’re lacking nurses, technicians, patient care assistants, transporters, and so many ancillary staff members. This increases the burden and responsibilities on the rest of us to do tasks that are outside of our purview — sometimes even unsafe for ourselves and patients — which then builds up resentment, burnout, and loss of dignity. There are several reasons for this lack of staff — the first is that our hospital refuses to hire more. As far as I know, the hospital lost millions and millions of dollars from the first wave of Covid-19, and since then it has been trying to recuperate its revenue and profits. One of the main ways it did that was by refusing to hire more nurses and other staff — and this was even before the Omicron surge. Other reasons are staff leaving due to vaccine requirements and also a high burnout rate leading to a large number of resignations. Medical residents such as myself often help nursing staff with patient care tasks because we know that the nurses are overwhelmed, but the flip side of that is that we become overwhelmed too — often having to stay late or fall behind in our other tasks because we’re helping with drawing blood, transporting patients, or even taking vitals.
Our hospital has money and will continue to have money, but its priorities are not in supporting its workers. Its priority is to create the image that we’re a premier hospital in New York City, at any cost. But the reality is that we’re not — lots of patients suffer because of the worker shortages and burnout. I’ve witnessed so many unsafe patient practices in my hospital because we don’t have enough trained people to distribute tasks responsibly or evenly according to ability. People are filling gaps where they can even if they are trained or not.
Omicron also made many of us sick. Many residents experienced symptomatic Covid-19, even if we were boosted, and called out of work. Our nursing colleagues also experienced outbreaks and called out. I remember that in my clinic, we only had two nurses to staff the entire clinic. I was helping them by taking the vitals for my patients and weighing them — a standard practice that nurses usually are responsible for in my clinic. But because of the shortage and the sick callouts, the responsibilities were shared to cover the shortage.
We’re repeatedly being told by my hospital that we have enough money to hire nurses and other staff but that it’s more of a “supply” issue than a “money” issue. Meaning that there are no nurses available to hire because of various reasons — burnout, relocation, retirement, etc. I verified this with some nursing colleagues (who are also associated with Left Voice), and they did corroborate that many healthcare workers have left the field during this pandemic, which makes sense. The hospital, though, is never short of resources to hire more staff where it can.
What is the state of healthcare worker burnout at your workplace?
We’re very burnt out. It’s so common that sometimes it doesn’t even phase us anymore. We are churned for our labor, go home, and do it again the next day. It’s deeply sad how working in health care robbed so many of us of our joy, even simple ones. One evening I was talking to a coworker about her plans after she completed her residency, and she said she just wanted to start reading books again. I won’t forget her response because it reminded me of how we can’t even do simple things that others may take for granted because our highly exploited working conditions leave us with little room to engage with life’s pleasures.
I felt I was very afraid that the Omicron surge would retraumatize people, and so I worked with some of my coworkers to set up support networks of care among ourselves, much like a mutual aid system. It is so easy to feel isolated and burnt out and [to feel that no one notices]. To prevent that, several of us came together to find more concrete ways to take care of each other through this surge. It’s the least we can do in solidarity for each other — especially when our bosses and administrators only care if we are well enough to work.
What are you and other residents and physicians demanding to keep yourselves and patients safe?
Unfortunately, I can’t share many specifics in order to protect our efforts and my coworkers.
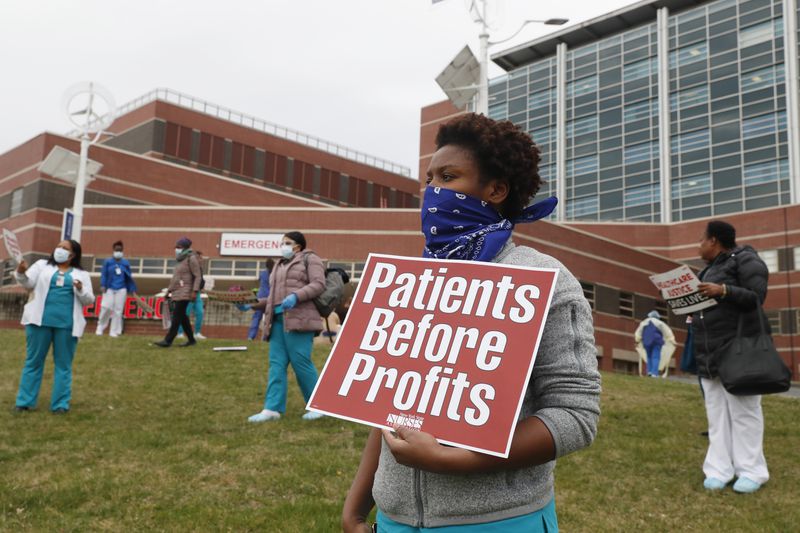
During the first wave, we built networks of solidarity among ourselves and drafted a long petition of demands to our hospital that were honored. This included hazard pay, childcare provisions, supplying adequate PPE, and decreasing barriers to PCR testing among hospital staff. We are still advocating for ourselves and our patients and will continue to do so.
Has your workplace instituted the CDC’s revised Covid-19 isolation measures, such as shortening the quarantine period or recommending that healthcare workers continue working even if they have Covid-19 but are asymptomatic?
Yes, my hospital has adopted this policy, much to the chagrin of residents like me. The fact of the matter is, you can still transmit Covid-19 even if you’re asymptomatic — and in a hospital setting, this puts a lot of fellow workers and patients at risk. Thirty percent of the Bronx is still not fully vaccinated — which means that there is a significant chance that asymptomatic hospital workers could transmit Covid-19 to a patient who, even if they’re vaccinated, can then potentially transmit the virus to someone they know who could not be vaccinated, or is immunocompromised, or elderly, or a child, or disabled, or a person with multiple chronic conditions.
What do you think of Biden’s messaging around the “pandemic of the unvaccinated”?
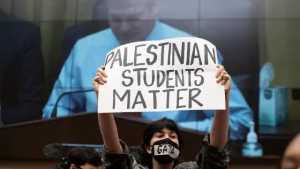
It’s nonsensical. It further asserts that the pandemic response is an “individual choice” issue rather than a collective response that the government could lead more effectively. We’ve drafted narratives that people are unvaccinated because they simply “choose” not to get vaccinated and that most of the anti-vaxxers are white, Republican Southerners. While some of this may be true, the reality is that the United States government, in its imperialist, neoliberal, and capitalist nature, failed so many people over so many decades that any systemic government response is not going to be trusted by many people. For example, there are still concerns about how vaccination rates differ in Black and Brown communities compared to white communities, a result of government pogroms that have targeted and exploited Black and Brown communities. White, working-class folks in the Midwest and South have been failed by the government, which decimated union rights and enabled mass poverty and dispossession in those communities. Why would anyone then trust the U.S. government about getting medical shots when the U.S. government can’t even provide basic life-supporting measures for its people — housing, food, water, wages, healthcare, education, etc? When it has repeatedly betrayed everyday people? This pandemic is not a “pandemic of the unvaccinated” — it’s a pandemic that has spiraled because of poor government policies and the history of capitalism, imperialism, and neoliberalism in the U.S. and its continued support of those principles today.
The Biden administration is trying to wash its hands clean by shifting the blame onto people rather than by examining its role in enabling the pandemic. It refuses to support global vaccine access, refuses to protect tenants against evictions, refuses to provide student loan debt relief, refuses to enact universal healthcare. All this contributes to exploding cases in the U.S. and mass death. It’s unsurprising that the U.S. exceeded 1 million positive Covid-19 cases in one day and that the pandemic continues to ravage communities.
The “pandemic of the unvaccinated” also implies that certain people are more valued than others, which is not true at all. Unvaccinated people deserve as much dignity and respect as vaccinated individuals, and rather than blaming them, it’s important to create a widespread culture of collectivity, solidarity, and care. The government is responsible for creating that culture and could lead that charge easily, but it doesn’t and it won’t.
What would a socialist response to the most recent Omicron surge look like?
It looks like many things. First, it looks like having a communist government, one that is run by the people with direct elections and the ability to recall representatives and set term limits. It looks like everyday people exhibiting ownership over their workplaces and making collective decisions over workplace conditions, revenue, and daily operations. It looks like providing free healthcare, housing, education, and basic income for everyday citizens. It looks like building a culture of solidarity and care. With regard to the public health realm, it means centering our response around our most vulnerable and not around profits, economic activity, or the most well. That would mean more enforced lockdowns, strict monitoring and enforcing of workplace safety measures, social distancing, and mask mandates. I say this because our most vulnerable — the elderly, disabled, immunocompromised, essential workers, those with multiple chronic conditions — have the most to lose if we are not serious or strict about our public health approach to the pandemic. A socialist response looks like global vaccine access, sharing vaccine technology and materials with other countries, lifting the blockade off Cuba, Iran, and North Korea. It looks like reckoning with the history of racism in the United States and offering reparations and material gains to Indigenous and Black and Brown communities. A socialist response looks like many things — it would center people over profits.
As a resident, do you have a message for other healthcare workers organizing for safe staffing, sufficient isolation lengths, and other protective measures to keep themselves, their coworkers, and their patients safe?
It is so, so important for my fellow coworkers to realize that we have more in common with each other than we have differences. Residency is viewed like a sprint — as in, worry about ourselves and get what we need to and leave. After all, it’s only three to five years of our lives. But it’s more than that — it’s actually a very traumatic time, especially during this pandemic. The hyperexploitation and trauma that comes from that never really leaves us. Even if our working conditions become better after we graduate and we may lose memory of it, the misery, isolation, and burnout that residency offers does have deep and subconscious effects on us.
Because of that, it’s important that we recognize that our working conditions bring us together in powerful ways even if we all have different backgrounds, material conditions, and trajectories. No one deserves to be exploited or powerless at work, and if we can organize around that, we can achieve many great things for ourselves.
I will also say that it’s important for my colleagues to recognize that other healthcare workers are not our enemies. Our enemies are the hospital and its leadership. Don’t blame nurses or other health care workers for having unions or fighting for their working conditions. They’re not doing it at our expense — in fact, we can learn a lot from them and organize with them to better our working conditions.
And lastly, be kind to yourself and those you work with. It’s hell out here, and the last thing we need is to beat ourselves or each other up.